The missing layer
between visits
Our MobiMed system connects our A3 wellness wearable and patient app to a cross-specialty EHR layer—with an AI-driven Guardian Layer that makes caregiver context permissioned, trusted, and usable.

Designed to fit seamlessly into daily life
Healthcare decisions are made with incomplete context.
Not because anyone is careless—but because day-to-day reality rarely makes it into care in a usable way. The result is guessing, delays, and preventable escalation.
Clinicians see patients briefly, then guess for months
Between visits, patterns shift (sleep, stress, symptoms, behavior)—but the care team often sees none of it.
Caregivers are invisible in the EHR
Parents, foster care, POAs, assisted living—they hold critical context, but lack a safe, structured way to contribute.
No shared, longitudinal view across specialties
Health data is fragmented across time, providers, and stakeholders—so teams can't easily see baseline vs. change.
Bottom line
When context is missing, care is slower, costlier, and more stressful—for patients, caregivers, and providers.
Three connected surfaces. One shared story.
Patients use it daily because it's easy. Caregivers use it because it's clear. Clinicians use it because it's actionable—embedded where they already work.
Patient experience: simple, consistent, low effort
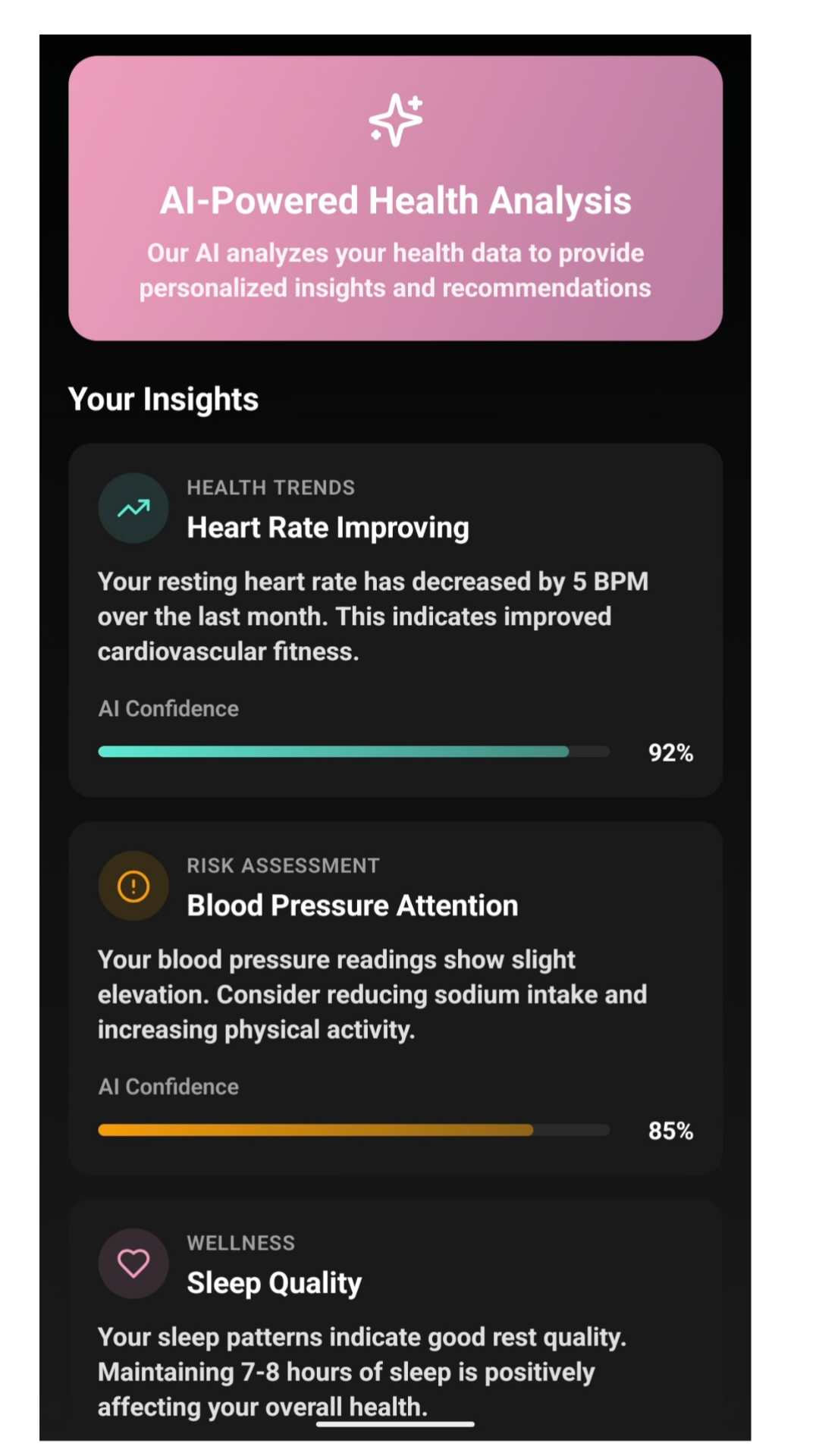
AI wearable + patient app
Voice-first, low-friction check-ins capture food, fitness, mood, symptoms, and vitals—without manual logging. Patients see simple trends and control what's shared.
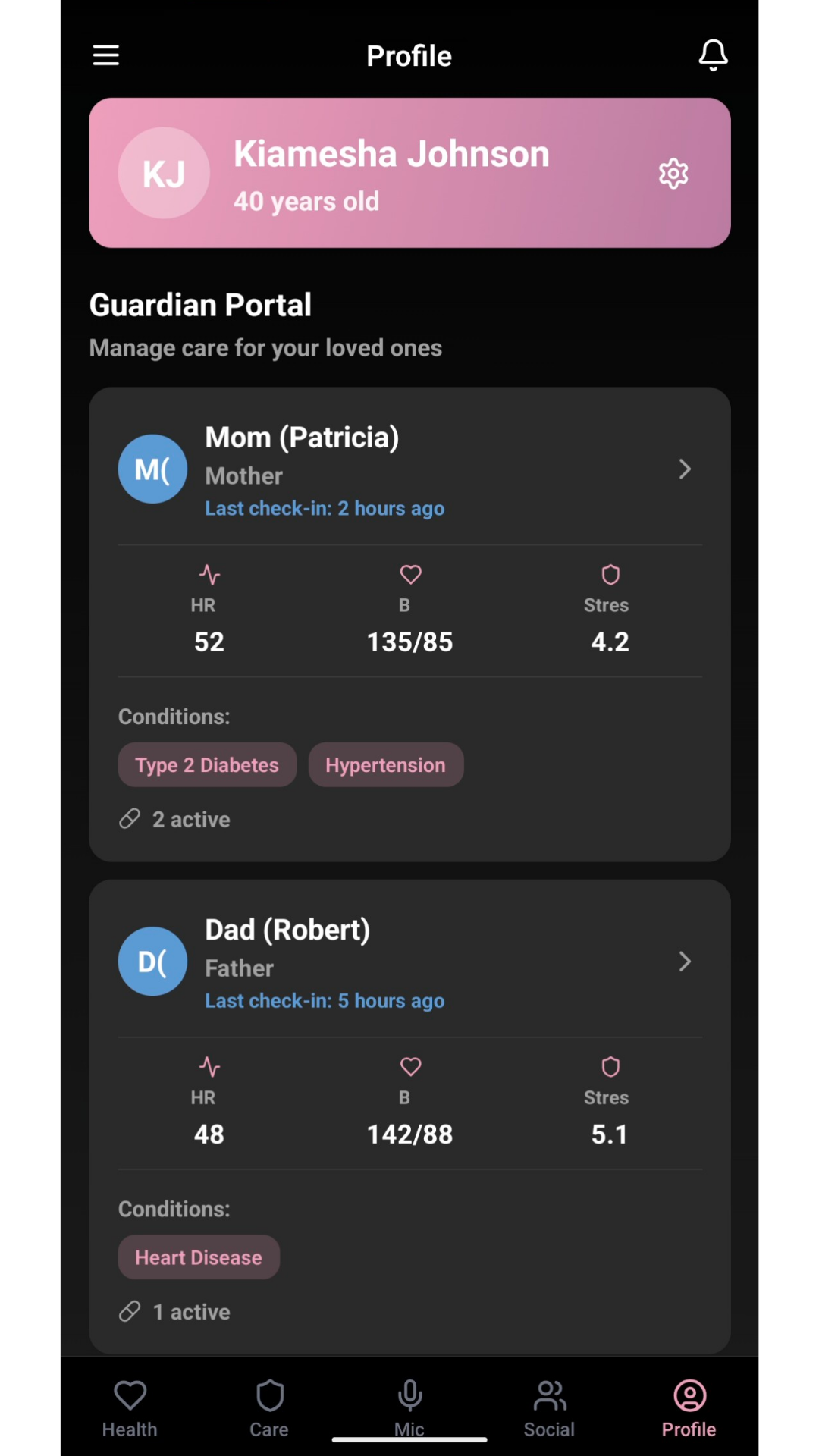
Caregiver experience: structured input with clear roles
Guardian Layer
Caregiving context is captured responsibly: parents, foster care, POAs, assisted living facilities can contribute observations with role-based permissions, time bounds, and auditability.
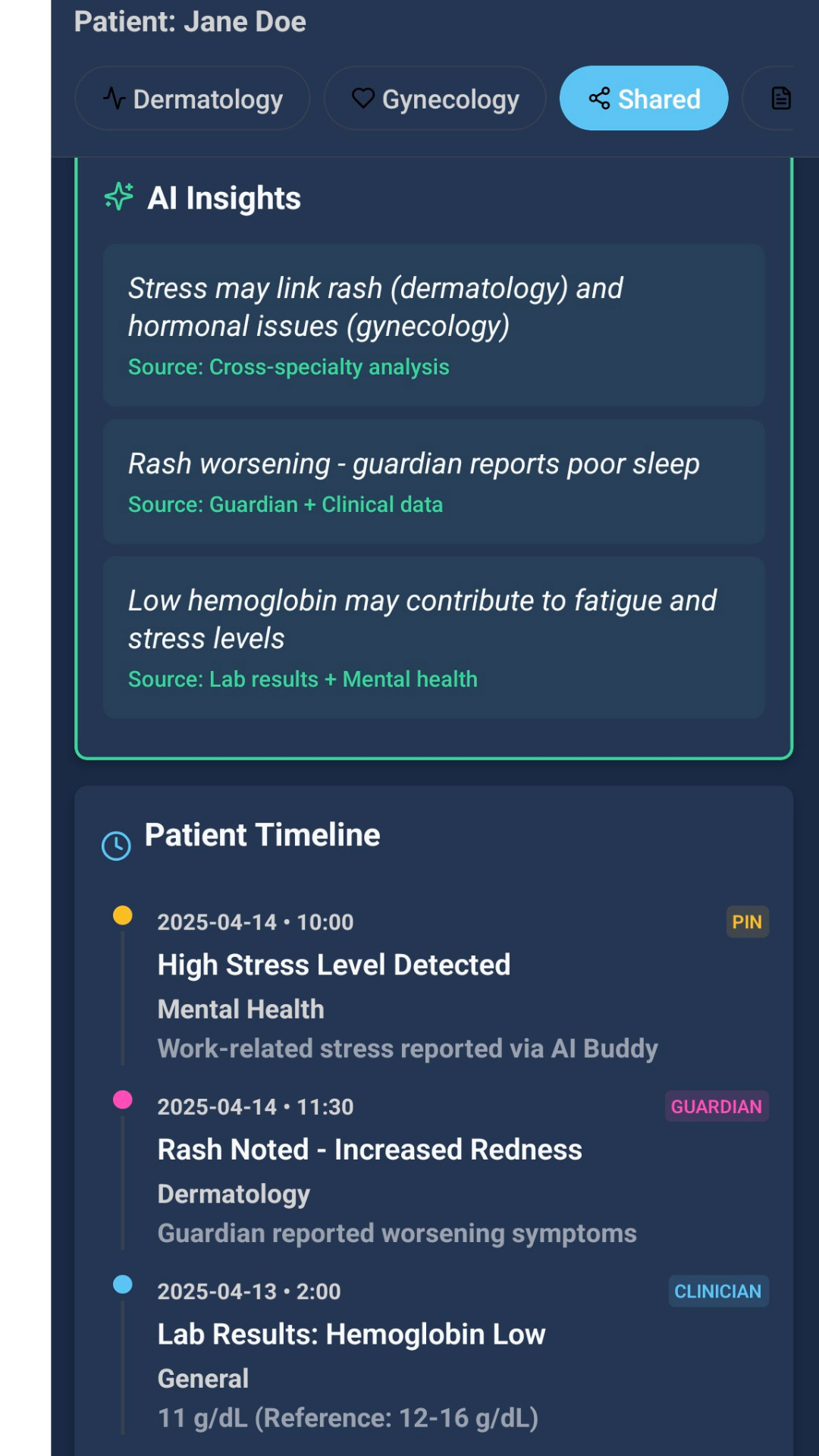
Clinician experience: actionable summaries inside workflow
Cross-specialty EHR view
A longitudinal, cross-specialty view shows baseline vs. change with source-tagged AI summaries and caregiver context—so teams can triage faster without noise.
Not more data—better signal.
MobiMed is designed to reduce guesswork and make care feel coordinated: for patients, for caregivers, and for clinical teams.
Earlier signal
Spot meaningful changes sooner with consistent between-visit context and baseline tracking.
Less burden
Patients don't have to "keep notes" or remember months of details—the story stays current.
Trusted caregiving
Caregiver input is permissioned, labeled, and auditable—so it helps rather than complicates care.
What this prevents
Delayed care, preventable escalation, redundant re-explanations, and caregiver frustration—caused by fragmented and missing context.
From daily life → to clinical clarity.
Designed for consistency, safe caregiving input, and clinician-ready summaries — embedded into workflows.
Patient checks in
Short voice check-ins + passive vitals capture: food, fitness, mood, symptoms, and trends.
Guardian adds context
Caregiver observations are submitted with role-based permissions, time bounds, and auditability.
AI summarizes change
Baseline vs. change is highlighted with source-aware summaries — not raw streams.
Clinician acts in-EHR
Teams see the longitudinal view where they work and can triage earlier with confidence.
The result
Clearer decisions, fewer surprises, and care that reflects real life — between visits, across people, and over time.
Why we built MobiMed
The beginning
Caring for someone you love is a labor of love—and it's also a lot to carry. 8 years ago, our co-founder Kiamesha Johnson began accompanying her grandmother, Nana Bea, to appointment after appointment as she managed multiple chronic conditions.
The confrontation
Nana Bea created a small booklet (which she always carried with her) that she called the "Refreshing Your Medical Memory Journal" to capture what happened after every visit and to keep her most updated health details. It worked—but it exposed a deeper truth: healthcare decisions were still being made with fragmented, incomplete context.
The resolution
In 2019, Kiamesha met her co-founder Lewis Goldsmith to reimagine that journal as a modern, shared system. The result became MobiMed—a connected experience for patients, caregivers, and clinicians designed to make between-visit reality visible.
Nana Bea passed away in 2023—but her journal became our mission.
Want to learn more?
Tell us who you are and what you’re exploring. We’re early and sharing what we’re building with investors and partners who want a closer look at the MobiMed system.”